Neonatology From A Parent's Perspective (895 Kb) by Dr Lindsay Craw is a focused summary of the research themes identified on parent perspectives and needs as they care for a sick child (baby in this case). Read to the end for 9 principles of family-centred care, as good a bullet point definition as I have seen.
Dr Craw explains she seeks 1. To understand the parental perspective of having an infant in the NICU 2. To consider how the experience may be unique for fathers and adolescent parents 3. To appreciate the financial burden families face 4. To look at end-of-life decisions from a parent’s perspective and 5.Suggestions for improving the parental experience.
She identifies sources of parent stress as Personal and family stressors, Prenatal and perinatal experience, Infant illness and appearance, Concern about outcome, Feelings of guilt, Sadness over a lost dream, Loss/alteration of parental role, Not getting to “know” the baby, Separation from their child, Alienation/sense of not belonging/loneliness, Being unprepared, Ineffective communication with healthcare providers.
Themes identified in the literature on parent's needs include:
1. “A need for accurate information and inclusion in the infant’s care
and decision making” - Parental distress was associated with receiving inaccurate and/or incomplete information - Contradictory information lead to confusion, decreased trust in the healthcare team and increased parental anxiety
2. “A need to be vigilant and watch over and protect the infant” - Wanted to oversee the infant’s care but as trust increased this watchfulness relaxed
3. “A need for contact with the infant”
4. “A need to be positively perceived by the nursery staff” - Feared being labelled as “difficult” and felt the need to conform to the “good mother” role
5. “A need for individualized care”
6. “A need for a therapeutic relationship with the nursing staff” – Mothers saw nurses as “gatekeepers” between themselves and their infants – Parents identified nurses as their primary source of information
Dr Craw also reviews literature on fathers, summarizing Johnson (2008) that:
• Most studies have looked at the experience of mothers
• Mothers need a sense of responsibility and control in caring for their infant
• Fathers need confidence in the health care team
• Loss of control was a major obstacle for some fathers
• Fathers have a sense of responsibility to return to work (coping mechanism)
• Without support and encouraging participation, fathers can become distanced from the family
• Fathers should be involved in hands-on care
•Ward (2001): Fathers ranked assurance and information needs as less important
than mothers but there were no differences in terms of comfort and proximity needs
A summary of Boss et al (2009)interviewed mothers under 21 to assess their understanding of the diagnoses, treatment and illness severity and who they spoke to from the medical team.
Results: 60% showed poor knowledge of either their infant’s illness severity, treatment or diagnosis – Greatest misunderstandings involved estimates of
illness severity – 46% of neonates were in “critical condition” but only
17% of mothers thought their infant was “very sick” – Adolescents who reported speaking with a physician were less likely to accurately assess the severity of
their infant’s illness (48 vs. 82% p=0.03) – Maternal age and educational level were NOT associated with improved knowledge of illness severity – Teens reported reluctance to ask health care providers to clarify technical language
Dr Craw also summarizes end-of-life decision making findings from Brinchmann et al. (2002):
• Wanted to be part of the decision making but not to make the final decision
• They felt they lacked the necessary medical knowledge and experience
• Doctors carry the responsibility of making the final decision
• Should be well-informed, listened to and if possible, told at a time when they are
ready to receive the information
• Wanted to be considered as individuals
• Parents have to live with the consequences of the decision
• Main concern was how doctors communicated with them and how the information
was presented
What is important to parents, in a nutshell?
• Continuity of care
• Individualized care
• Consistent and effective communication
• Relationships with healthcare providers
• Parental involvement
• In a study by Reid et al. (2007): – 36% of parents could not identify a staff
person whom they felt they could talk to - 25% felt they could not ask too many
questions – 29% identified a lack of privacy which stopped them from having discussions with the staff
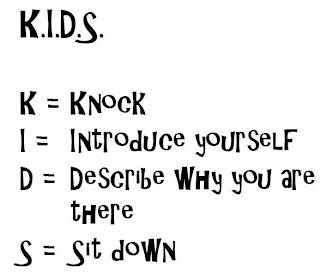
Weiss (2009) reviewed a targeted intervention that improved the satisfaction of parents with provider communication. The intervention included (1) Education module for medical providers, (2) Contact card for parents with medical providers names, job descriptions and contact information, (3) Poster of faces, names and titles of medical providers on display at the entrance.
Dr Craw defines Family Centered Care as “Acknowledging he central role that the family plays in a child’s life and incorporating practices, policies and programs that support the family”. 9 principles of family-centred care include:
1. Recognizing the family as a constant in the child’s life
2. Facilitating parent-professional collaboration
3. Honouring racial, ethnic, cultural and socioeconomic diversity
4. Sharing complete and unbiased information on a continuous basis
5. Responding to the child and family developmental needs as part of healthcare practices
6. Encouraging and facilitating family to family support and networks
7. Adopting policies and practices that provide families with emotional and financial support
8. Designing healthcare that is flexible, culturally competent, and responsive to families
9. Recognizing family strengths and individuality and respecting different methods of coping